Understanding the Difference and Similarities Between CRISPR Gene Editing and Epigenome Editing
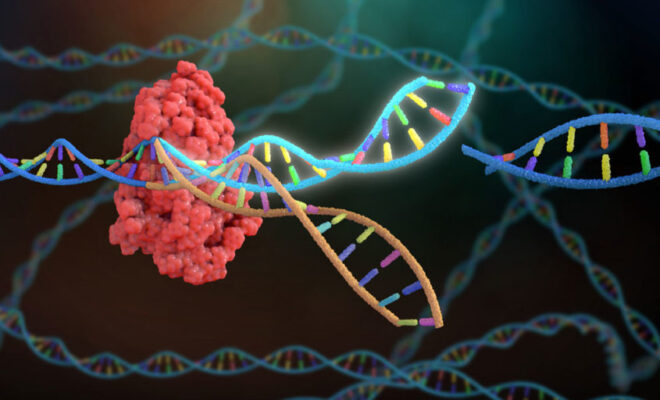
Since 2012, when genetics scientists Jennifer Doudna and Sam Sternberg published their findings in Nature on Clustered Regularly Interspaced Short Palindromic Repeats, CRISPR has become a promising new tool to help medical researchers devise genetic diseases for disorders. You use CRISPR to make changes to living cells in humans, with the idea that you can address problems coming from mutations and inherited conditions.
There is a new approach gaining a foothold in research institutions to edit DNA, known as epigenomic editing. It’s useful to become familiar with the similarities and differences of epigenomic editing and CRISPR gene editing.
Compare CRISPR Gene Editing and Epigenomic Editing
Changes that scientists make using DNA editing are permanent, which means that you want to be as certain as possible that you aren’t introducing any potentially bad effects that would be difficult or impossible to reverse.
But according to Science, “epigenomic edits might be less likely to cause harmful off target effects and can be reversed. They can also be more subtle, slightly ramping up or down a gene’s activity, rather than blasting it at full force or erasing it altogether.”
DNA editing can enable a protein to turn on a genetic sequence or suppress an unwanted gene. Using cancer therapies that rely on this approach can be imprecise, so multiple genes are affected simultaneously instead of just the one that the doctor wants to target, potentially resulting in dangerous side effects.
With epigenomic editing, though, the changes scientists make can be more precise as well as reversible. Epigenomic editing employs the same enzymes used by cells to activate and deactivate their genes. This allows for more efficiency and versatility. You can use one gene editor to suppress a particular portion of the genetic code and another editor to activate a gene.
An example of an attempt at epigenomic editing is from Sangam Therapeutics. About 20 years, ago, this biotechnology company was working on the VEGF gene, which is responsible for promoting the growth of blood vessels.
The company wanted to make a therapy to bring back blood flow in people suffering from diabetic neuropathy (nerve damage). But injecting the edited genes into leg muscles wasn’t an effective way to deliver the needed therapy. As a result, the scientists harnessed a harmless adeno-associated virus (AAV), forcing the cell to use it to make a reliable supply of proteins. Now, the company is using it to reduce the tau protein, which is implicated in Alzheimer’s disease and Huntington’s disease.
Other researchers, according to Science, are using AAV approaches to improve protein expression in treating a form of obesity that people inherit from their parents. Then, there is work proceeding with epigenomic editing to battle Dravet syndrome, which is a kind of epilepsy with severe symptoms.
A Look at Epigenomic Editing
Scientists typically use a “dead” or inactive form of the Cas9 CRISPR protein to target a particular gene in question. Then they use an effector protein to remove or add chemical tags to DNA and the histone proteins, to cause genes to express or to inhibit their expression. AAV approaches have drawbacks in that they are often expensive to use.
What’s more, their use can cause patients to have an adverse immune system response. And it’s not a permanent change since as cells divide, the encoding of DNA done with the epigenomic editor will erode over time.
A new approach, per Science, comes from Angelo Lombardi and colleagues at the San Raffaele Telethon Institute for Gene Therapy. He announced at the May American Society of Gene and Cell Therapy meeting in Washington, D.C., that they have created a “cocktail” using three separate epigenomic editors to repress gene expression in a petri dish, whose effects did persist even after the cells continued to divide.
It raises the idea of using lipid nanoparticles to deliver the protein as messenger RNA to cells, so they will only produce the protein for a limited period, making them less likely to provoke a strong immune system response.